Endoluminal or Subintimal?
Endoluminal or subintimal recanalization? Practical guide to choosing the right approach for chronic total occlusions based on lesion length, vessel calcification, and anatomy — with evidence-based insights from daily endovascular practice.
How to choose the right path to reach your destination
There are still few shared rules and no universally accepted algorithm to guide the choice between endoluminal and subintimal recanalization.
Despite decades of experience and countless attempts, only limited evidence has emerged on when to stay inside the true lumen and when to go off-road.
It’s a difficult goal to achieve – standardizing what, by nature, depends on anatomy, operator experience, and, ultimately, intuition.
While waiting for future studies to put order in this uncertainty, I’ll share here some personal reasoning – born from daily experience and supported, where possible, by the literature...
1. The length of the occlusion
In my personal experience, an endoluminal attempt is usually easier and more effective in short occlusions.
But what does short really mean?
In practice, I consider “short” any chronic total occlusion (CTO) under 10 cm in length.
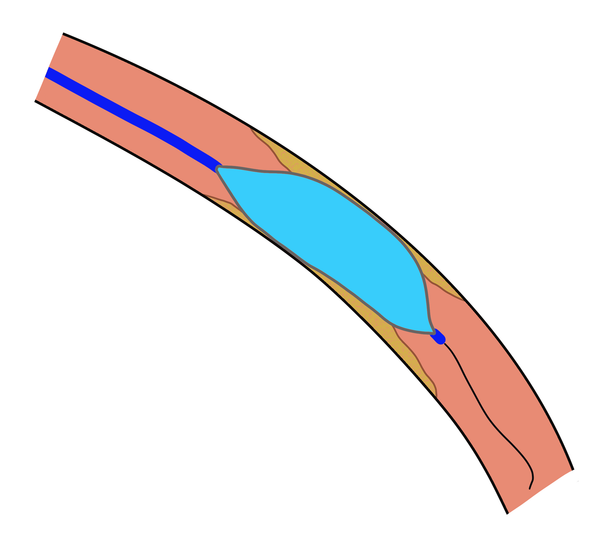
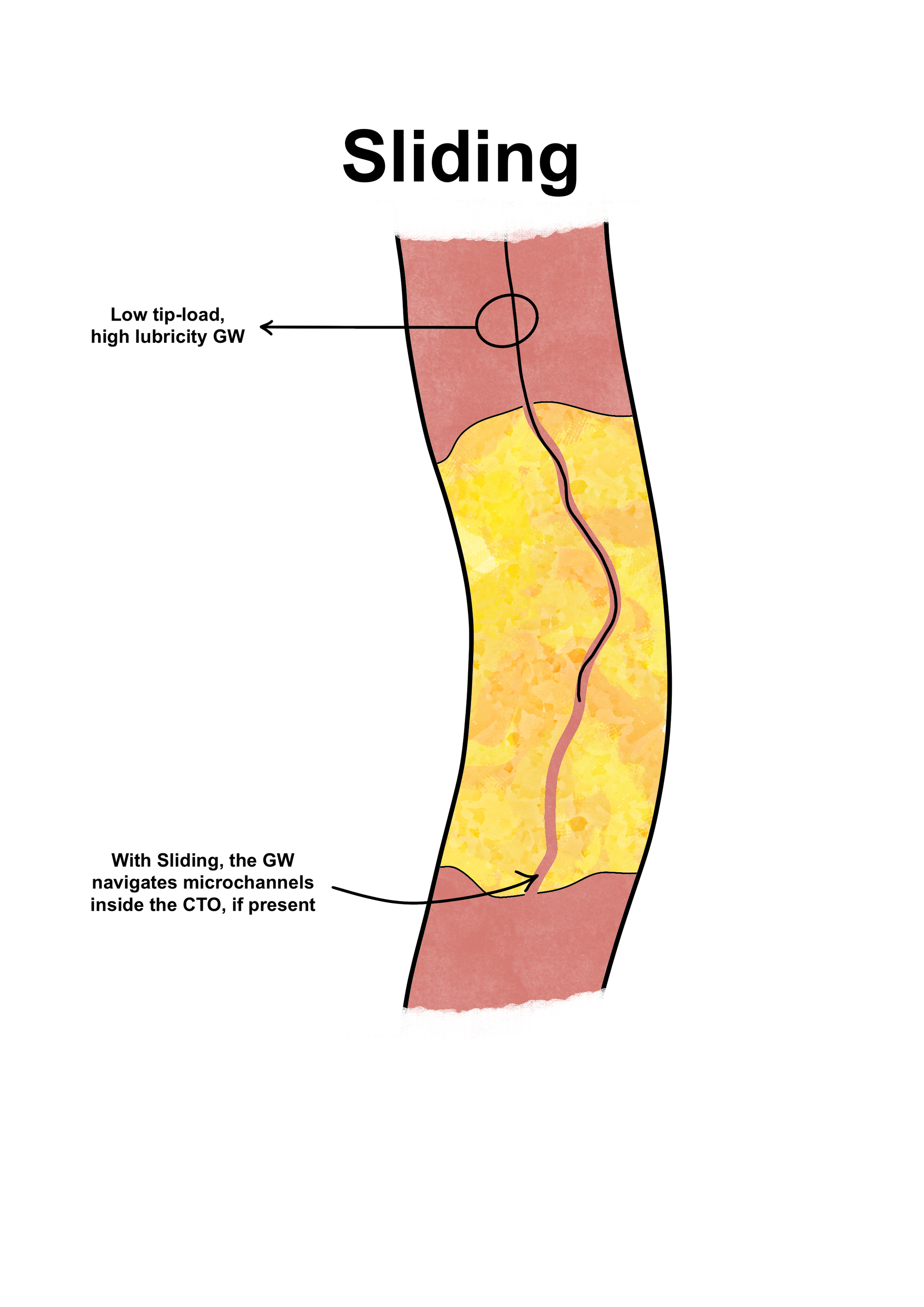
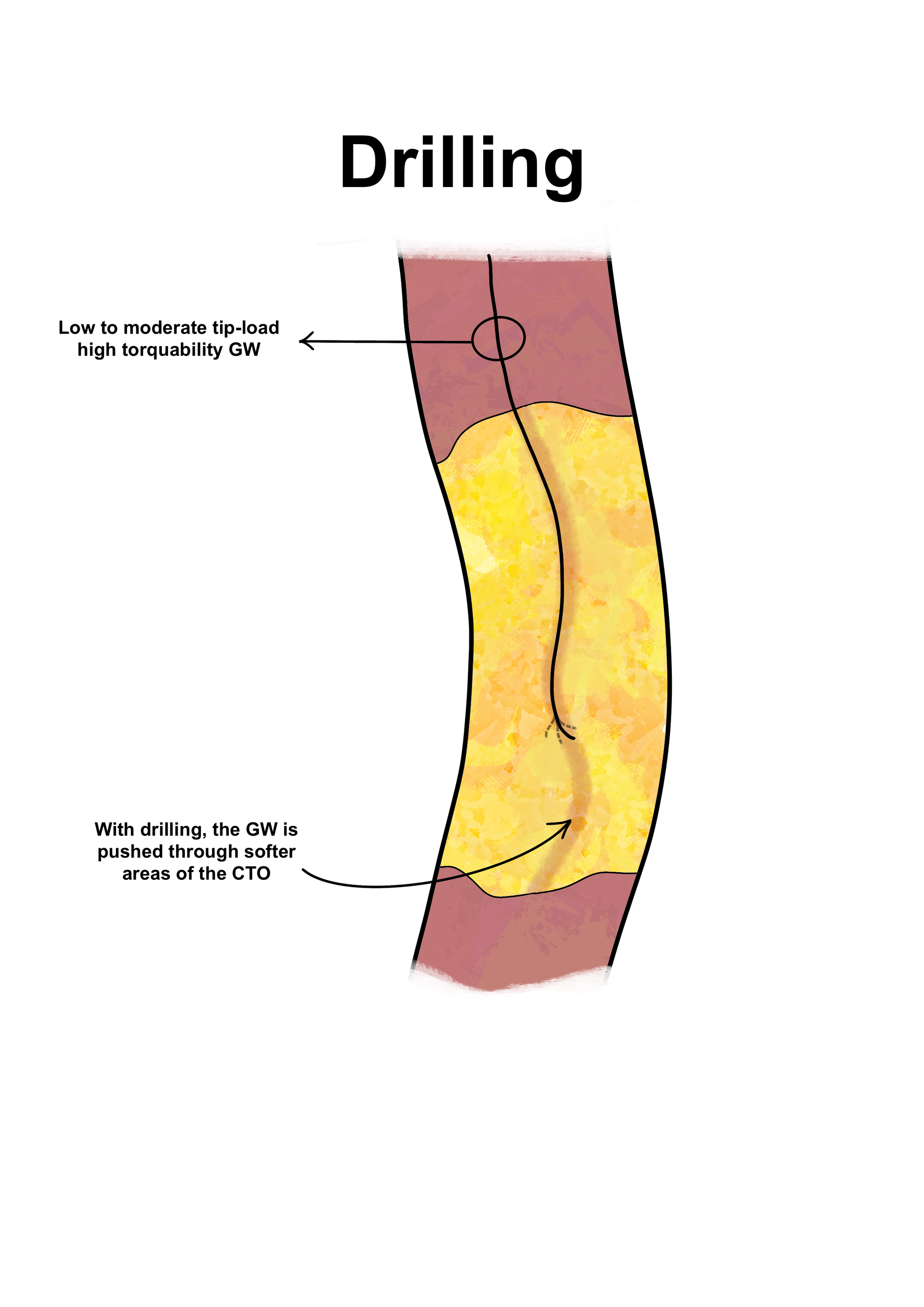
These lesions, especially when located in the femoro-popliteal segment, are often successfully crossed endoluminally using the drilling or sliding techniques.
The perforating technique, on the other hand, should be reserved for even shorter lesions, and only when they lie in straight vessel segments.
Attempting a perforating approach in a tortuous or curved segment, such as the ostium of the anterior tibial artery, increases the risk of vessel perforation.
That’s because, by its own nature, the wire in this technique advances in a linear trajectory, regardless of the vessel curvature.

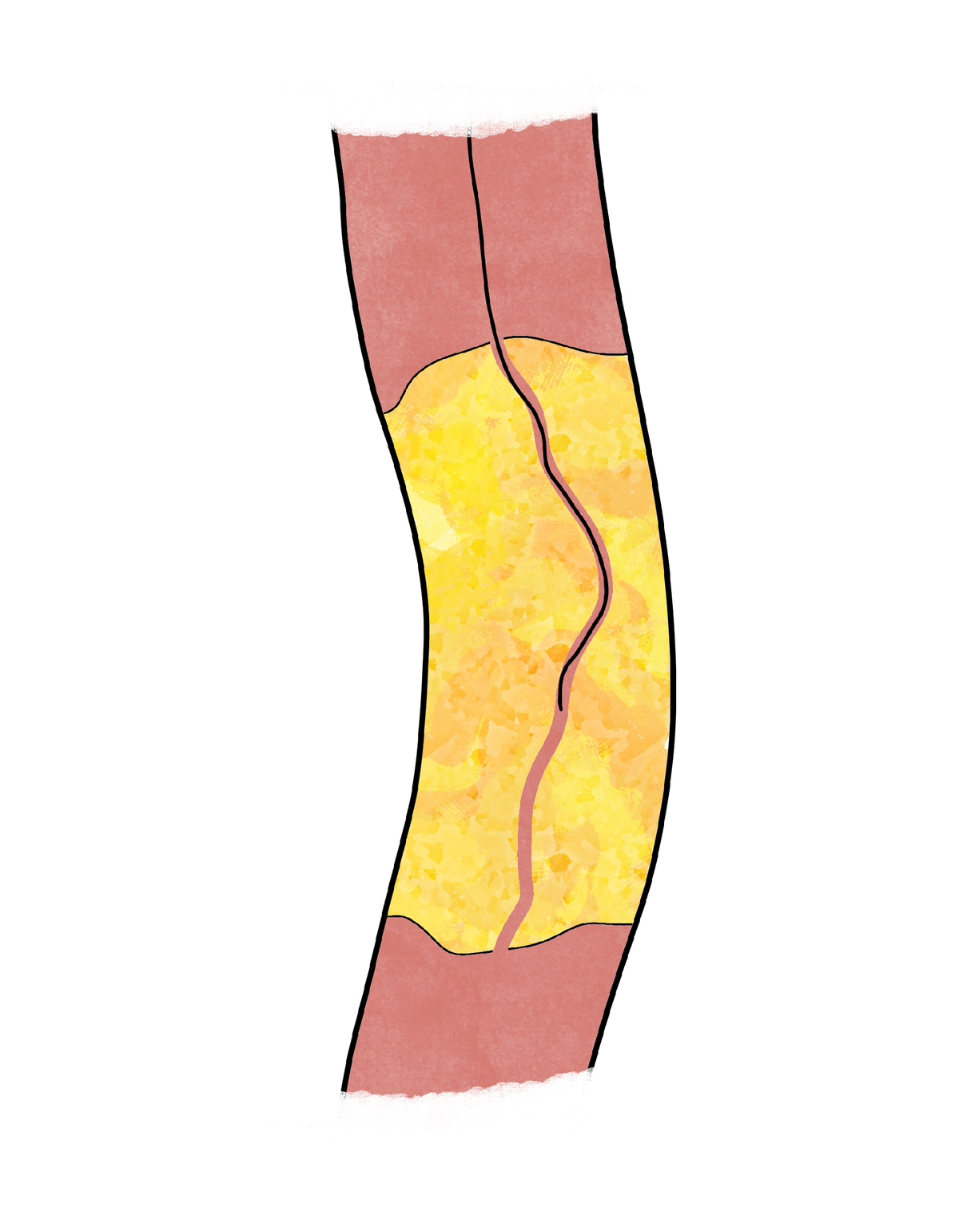
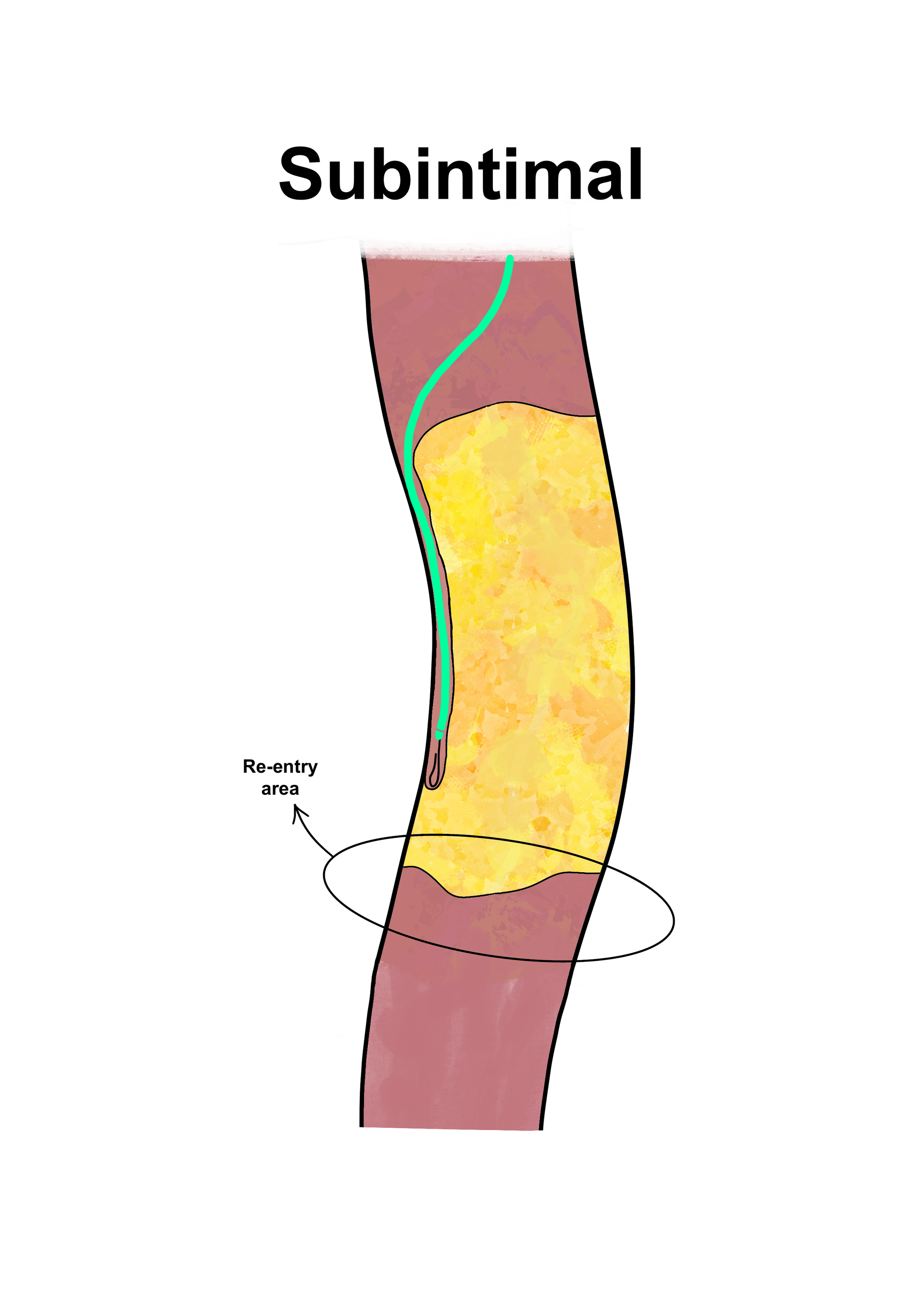
Longer and more complex lesions – those exceeding 20 cm – are usually recanalized through a subintimal approach.

In these cases, selecting the re-entry zone is critical. As is well known, it needs to be as close as possible to the distal cap of the CTO, in order to preserve the distal collateral network that often emerges near the point where the true lumen reopens.
Medium-length CTOs (between 10 and 20 cm) define a hybrid territory where either an endoluminal or subintimal approach may work, depending also on the composition of the lesion.
2. The quality of the arterial wall
Where severe calcification of the wall is present – particularly in diabetic or dialysis patients – I tend to avoid a subintimal approach whenever possible.
In my experience, medial calcification (also called Mönckeberg sclerosis) makes distal re-entry extremely difficult, sometimes nearly impossible. The wall becomes an uncrossable obstacle. Literature supports the finding of a difficult re-entry in this scenario, even with the use of re-entry devices.
Therefore, the endoluminal pathway would be my choice in this scenario whenever possible.
Similarly, fresh thrombotic occlusions – either acute thromboses or thrombosis on plaque – are typically easy to cross endoluminally, though they carry a high risk of distal embolization during angioplasty.
So, in these situations – after successful crossing of the fresh occlusion – mechanical thrombectomy or primary stenting should be considered as safer and more effective revascularization options than standard POBA.
3. The anatomical district
The vessel’s location also dictates the strategy.
Whenever the preservation of collateral circulation is essential, the endoluminal approach should be prioritized.
A clear example is the pedal-plantar loop.
When performing a recanalization – not merely a navigation – of this region, a subintimal approach can destroy the inter-digital collateral network – which is crucial to maintaining the hemodynamic stability of the foot and, ultimately, limb viability.
Another critical zone is the popliteal trifurcation.
When a popliteal occlusion reaches the trifurcation and the emergence of tibial or peroneal branches is visible, maintaining an endoluminal route – or, when necessary, attempting a retrograde approach – is often the best way to preserve the bifurcation’s integrity.
Subintimal crossing can be an option in extreme, otherwise uncrossable cases – provided that re-entry isn’t too distal and doesn’t jeopardize the emergence of tibioperoneal branches at this level.
A matter of anatomy, not ideology
The choice between endoluminal and subintimal is not a matter of preference but of correct strategy and proper reading of context.
Daily practice and the grind often push us to treat vessel morphology almost instinctively – and to let the wire find the easier path through the vessel. But sometimes our eyes and mind need to move beyond and faster than our virtuous hands.
The difference between Pat Metheny and any other indistinct, ultrafast and even famous jazz musicians lies in one single fact: beyond his astonishing technique, he uses his brain more than his fingers.
Probably the repeated execution of the “first think – then move your hands” pattern will come to our aid with time. Like driving a car, the more you’ve driven it, the more naturally you sense what the correct handlings are to apply while driving.
With time, that decision – endoluminal or subintimal – becomes less about theory and more about perception.
Let’s open the discussion
How do you decide when to stay on path and when to go off-road?
I’d love to read your perspective, your personal rules, or even your doubts.
Share your experience in the comments below — let’s make this one of those topics where conversation precedes consensus.
Previous Posts | About | Manage Account
References:
Kim K, Ko YG, Ahn CM, et al. Clinical outcomes of subintimal vs. intraluminal revascularization approaches for long femoropopliteal occlusions in a Korean multicenter retrospective registry cohort. Circ J. 2018; 82(7): 1900–1907. doi:10.1253/circj.CJ-17-1464.
Tsitsiou Y, Ekpe J, Harris L, et al. Use and effectiveness of Pioneer re-entry device for subintimal true lumen re-entry: single-centre data and a review of the literature. CVIR Endovasc. 2021; 4: 81. doi:10.1186/s42155-021-00268-w.
Tomoi Y, Takahara M, Kuramitsu S, et al. Subintimal versus intraluminal approach for femoropopliteal chronic total occlusions treated with intravascular ultrasound guidance. J Am Heart Assoc. 2021;10(20): doi:10.1161/JAHA.121.021903.